Ethics Direct and Ethics+ Services
Medical Ethics

Ethics is a philosophical discipline pertaining to notions of good and bad, right and wrong—our moral life in community. Bioethics is the application of ethics to the field of medicine and healthcare.
Ethicists and bioethicists ask relevant questions more than provide sure and certain answers.
Health care ethics (aka “medical ethics” or “bioethics”), at its simplest, is a set of moral principles, beliefs and values that guide us in making choices about medical care. Our sense of right and wrong and our beliefs about rights we possess and duties we owe others are at the core of health care ethics.
The four basic principles of bioethics are:
- Autonomy: to honor the patients right to make their own decision
- Beneficence: to help the patient advance his/her own good
- Nonmaleficence: to do no harm
- Justice: to be fair and treat like cases alike
These resources provide education, guidance and examples of those principles in action.
Ethical Issues in Healthcare of Persons with Developmental Disabilities
A Threat to Disabled Persons?
On the Genetics Approach to Developmental Disabilities
This essay by Hans S. Reinders explores the claim that the genetics approach to intellectual disability does not imply a negative evaluation of disabled persons because there is a distinction between the person and the condition.
Being Human:
Issues in Sexuality for People with Developmental Disabilities
Discussion of sexuality issues in the lives of persons with developmental disabilities has been neglected by both the general public and professionals for many years. Despite philosophical shifts that have focused on improved community living and quality of life, most people in the field of developmental disabilities have ignored the central issues of sexuality and sexual expression.
Proponents of Quality of Life assessment often link QOL with contentment, a fact that many result in interference of the rights of people with disabilities. Instead, the voices of the client, his or her caregivers, and of society at large need to be listened to and respected.
Shared Decision Making: The Ethics of Caring and Best Respect
Making decisions regarding life-sustaining treatments for patients who are severely disabled involves some of the most difficult clinical dilemmas in bioethics. This paper focuses on two aspects of this kind of decision making: 1) accurately determining a mentally disabled patient’s decision-making capacity, and 2) making treatment decisions for patients who have never had or who do not currently have decision-making capacity and have no available surrogate.
Silences by Theodore J. Dibuon, MD
The silences are eloquent…
This is an account of how one young man, born with a disability, took control over his own health care decision making.
Research
The Center can support your efforts in protecting human subjects, including service on Institutional Review Boards and non-scientific review panels and learning health system activities.
Moral Distress
Moral Distress in Healthcare
The sense that one’s work may be compromising, or even corrupting, is common, with the experience among nurses especially severe.
Freda’s Wishes
Freda is a 32-year old woman in an advanced stage of multiple sclerosis, no longer able to move independently or to feed herself. Is a feeding tube the answer?
Moral Distress or Moral Comfort
Moral distress in healthcare results from a professional’s inability to provide compassionate care to patients because of individual, organizational, or societal barriers. Research suggests that moral distress is a growing concern among nurses and may be a major reason why nurses leave one job for another or abandon the profession of nursing.
In the Patient’s Best Interest – A Call to Balance
Nurses, physicians, and other healthcare professionals often complain that a loss of freedom or other obstacles hinder their ability to act in the best interest of the patient. These barriers cause professional burnout and moral outrage and may contribute to a migration away from healthcare.
Moral Fatigue – A Nursing Perspective
It seems inevitable that a phenomenon called moral fatigue would be labeled, described, and applied to nurses, whose working environment has more than its share of moral conflicts. This article explores the dimensions of moral distress among nurses and presents moral fatigue as a holistic experience with both personal and institutional consequences.
Virtue, Foible and Practice – Medicine’s Arduous Moral Triad
Moral distress is often discussed as a response to the moral dilemmas that professional and other caregivers encounter in their effort to balance competing moral principles, or to provide care in difficult cases, to difficult patients, in spite of difficult institutional requirements or policy. In this essay, a reforming ER clinician and teaching physician, offers a personal approach to moral distress.
Moral Distress – The Role of Ethics Consultation in the NICU
Moral distress is a common occurrence for individuals involved in the care of critically ill infants. The ability to reason through difficult situations is often complicated by intensely emotional circumstances. Ethics consultation in the Neonatal Intensive Care Unit is a useful tool for caregivers and families who face moral problems.
Organizational Ethics
From Clinical to Organizational Ethics – The Second Stage of the Evolution of Bioethics
Patient Rights and Organization Ethics – The Joint Commission Perspective
Individuals Bear Responsibility
Organizations, Ethics and Health Care – Building an Ethics Infrastructure for a New Era
The Evolving Health Care Marketplace
Hospital Mergers and Acquisitions – A New Catalyst for Examining Organizational Ethics
Benefits of Ethics Services
Improved employee retention / performance and reduced stress
Improved health outcomes / patient satisfaction
Increased compliance and safety
Proactively manage risk
The Joint Commission / Accrediting Body

Clinical Care/Patient Outcomes
Risk Management
Quality Improvement
Compliance & Safety
Human Resources & Professional Development
Mission Effectiveness
Clinical Care/Patient Outcomes
Risk Management
Quality Improvement
Compliance & Safety
Human Resources & Professional Development
Mission Effectiveness
Improve Ethics Performance
The CPB ethicist helps build internal organizational ethics capacity over time. As advisory support decreases with internal competency, consultation services increase and overall ethics performance improves.

Choose the Service That's Right for You
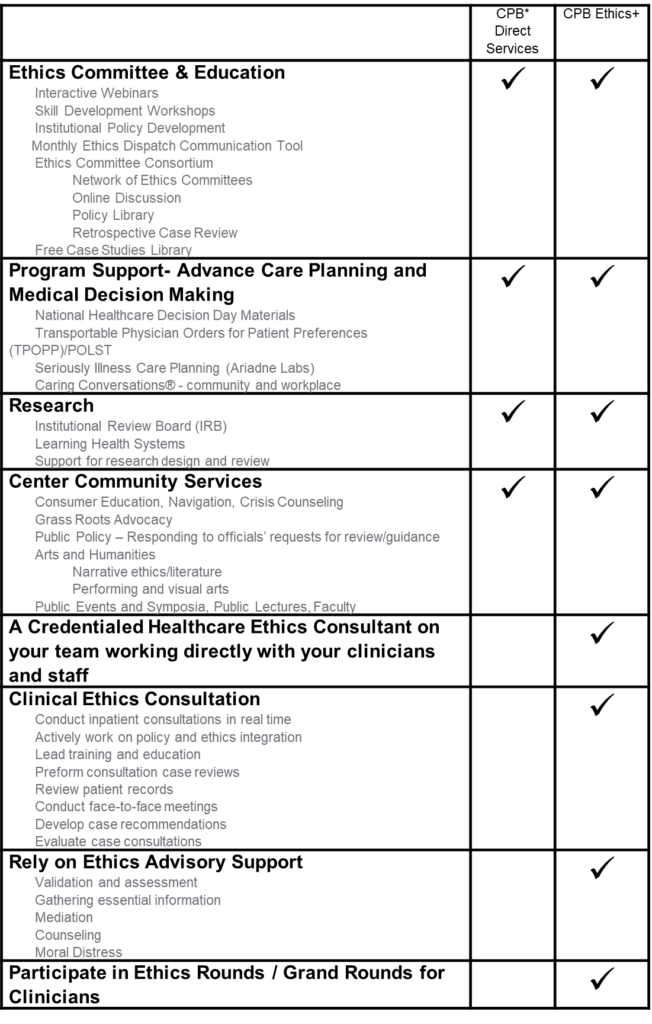
* CPB: Center for Practical Bioethics
Included in Your Ethics Services:
Ethics Dispatch and Ethics Committee Consortium
Monthly Ethics Dispatch
The Center’s monthly Ethics Dispatch fills the skill development needs of health professionals and providers from mid-career volunteers to new students. Each issue focuses on a particular topic relevant to the field of medical ethics, addressing it from different approaches and perspectives.
The goals:
• Educate and elevate the effectiveness of Ethics Committees and their members
• Furnish a turnkey resource for Ethics Committee leaders, challenged with daily routines, allowing little time for content development.
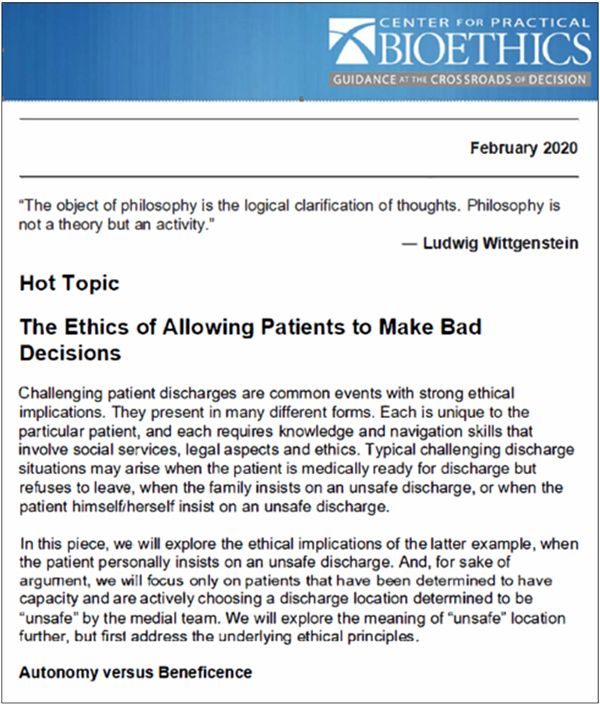
The Ethics Dispatch includes four educational elements, each addressing the monthly topic in different ways:
Hot Topic – The Center’s clinical ethics staff focus on an ethical issue impacting providers regionally or within the field while providing guidance. This is a researched deep dive that frames the issue in understandable language from an industry perspective with practical recommendations. Previous issues have addressed a range of concerns, from life-saving interventions following suicide attempts to public health concerns due to anti-vaccination decisions.
Bioethics in the News – Web links to the most recent and relevant stories in the news pertaining to issues of concern for ethics committee members.
Case Study – Each issue includes a case study that illustrates the topic of the month in a real-life situation.
Ethical Musings – In this section, the author takes a more personal approach to presenting the underlying philosophical insights relevant to the monthly topic. This is presented through a philosophical framework based on arguments to add deeper understanding of the clinical ethics topic.
For More Information About Ethics Services
Ryan Pferdehirt, D.Bioethics, HEC-C
DIRECTOR OF MEMBERSHIP AND ETHICS EDUCATION
rpferdehirt@practicalbioethics.org
816-979-1350
Featured Resources
Receive More Information
Make Impact
Every dollar you give helps, providers, clinicians, patients and families
decide what to do when it’s hard to agree about the “right” thing to do.








